The joyous arrival of a newborn can sometimes be overshadowed by a life-threatening complication: postpartum hemorrhage (PPH). This event, characterized by excessive bleeding after childbirth, requires swift and decisive action from healthcare professionals. A comprehensive nursing care plan for PPH is essential to ensuring the safety and well-being of mothers.
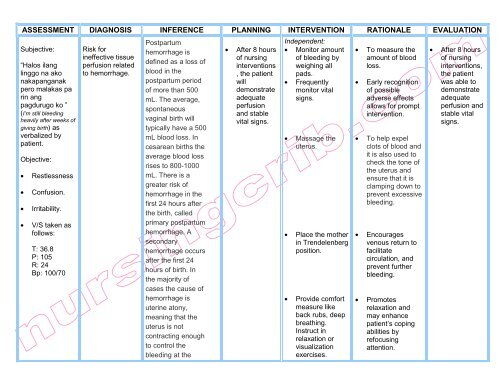
Image: www.vrogue.co
This article delves into the intricacies of postpartum hemorrhage, exploring its causes, risk factors, and the vital role nurses play in managing this critical condition. We will navigate the multifaceted aspects of nursing care, encompassing assessment, intervention, and monitoring, all aimed at achieving a positive outcome for mothers and their newborns.
Understanding Postpartum Hemorrhage: A Closer Look
Definition and Epidemiology
Postpartum hemorrhage (PPH) is defined as blood loss exceeding 500 ml after vaginal delivery or 1000 ml after cesarean delivery. It is a leading cause of maternal mortality worldwide, accounting for a significant portion of maternal deaths. The World Health Organization (WHO) estimates that about 14% of women experience PPH globally.
Causes of Postpartum Hemorrhage
The underlying causes of PPH can be categorized into four main groups:
- Uterine Atony: This is the most common cause, occurring when the uterus fails to contract properly after delivery, resulting in continued bleeding.
- Genital Tract Lacerations: Tears in the cervix, vagina, or perineum can lead to significant blood loss, especially if they go undetected.
- Retained Placenta: When the placenta does not fully detach from the uterine wall, it can cause continued bleeding.
- Uterine Inversion: A rare but serious condition where the uterus turns inside out, often triggered by excessive cord traction or strong uterine contractions.
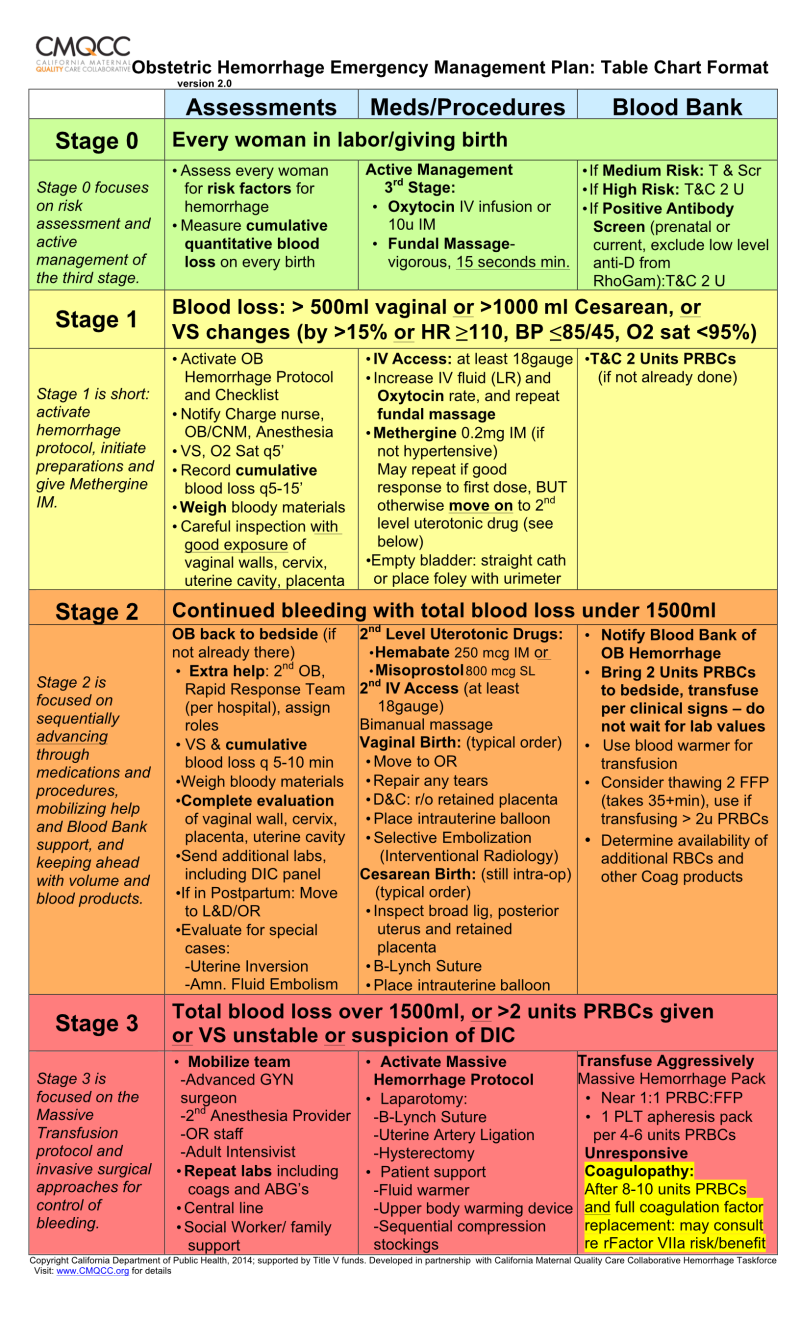
Image: mungfali.com
Risk Factors for Postpartum Hemorrhage
Several factors can increase a woman’s likelihood of developing PPH:
- Previous Postpartum Hemorrhage: History of PPH significantly elevates the risk of recurrence.
- Multiple Pregnancies: Women who have had multiple pregnancies are at greater risk due to uterine stretching.
- Rapid Labor and Delivery: Fast deliveries may not allow enough time for the uterus to contract adequately.
- Large Birth Weight: Babies with larger birth weights can put more strain on the uterus.
- Induced or Augment Labor: Medical interventions such as labor induction or augmentation can increase the risk of uterine atony.
- Placenta Previa or Abruptio Placentae: These placental complications are associated with an increased chance of PPH.
- Obesity: Women with obesity are at higher risk of PPH due to factors such as increased blood vessel size.
- Chorioamnionitis: Infection of the amniotic sac, a complication of pregnancy, can also increase the risk of PPH.
The Crucial Role of Nurses in Managing Postpartum Hemorrhage
Nurses play a vital role in the prevention, early detection, and management of PPH. This requires thorough knowledge of risk factors, early assessment, timely communication, and skilled interventions.
Assessment and Monitoring
A meticulous assessment and continuous monitoring are vital for recognizing and responding to PPH promptly. Nurses should:
- Monitor Vital Signs Regularly: Closely observe blood pressure, pulse, respiration, and temperature, which can be altered in PPH.
- Assess Estimated Blood Loss: Estimate the amount of blood loss by observing the saturation of pads, linens, and the collecting basin.
- Inspect the Vagina and Perineum: Examine for lacerations, hematomas, or other signs of bleeding.
- Palpate the Uterus: Regularly assess uterine tone and position by gently palpating the abdomen. A soft, boggy uterus is a prime indicator of atony.
Interventions and Nursing Care
Nurse-led interventions are central to addressing PPH effectively:
- Fundal Massage: This technique stimulates uterine contractions, helping to reduce bleeding.
- Uterine Tamponade: Inserting a balloon catheter into the uterus can help control bleeding by applying pressure on the uterine wall.
- Fluid Replacement: Intravenous fluid administration is crucial to maintaining hemodynamic stability in cases of blood loss.
- Medication Administration: Oxytocin, a potent uterine stimulant, is often used to induce contractions and reduce bleeding. Other medications like methylergonovine or carboprost are also used to control bleeding. Nurses are responsible for ensuring accurate administration and monitoring for potential side effects.
- Blood Transfusion: If the patient experiences significant blood loss, blood transfusions may be necessary to replenish blood volume. Nurses play a vital role in preparing and monitoring blood transfusion procedures.
Collaborative Care
Effective care for PPH requires a collaborative approach involving nurses, physicians, and other healthcare professionals. Nurses communicate findings and concerns to the physician, coordinate orders, and provide ongoing updates on the patient’s condition. They also play a crucial role in ensuring the patient’s comfort and safety.
Preventing Postpartum Hemorrhage: Proactive Care
While PPH is not always preventable, certain actions can significantly reduce the risk:
- Early Recognition of Risk Factors: Identifying women at risk for PPH during pregnancy allows for proactive measures.
- Active Management of the Third Stage of Labor: Close monitoring of the third stage of labor, which involves the delivery of the placenta, is essential for detecting and managing any complications early. Practices like controlled cord traction and prompt administration of oxytocin after delivery can help prevent atonic bleeding.
- Appropriate Use of Medications: Strategic use of medications like uterotonics can help prevent or manage uterine atony.
- Access to Skilled Healthcare Providers: Ensuring that women have access to qualified healthcare professionals who are equipped to manage PPH emergencies is crucial.
Nursing Care Plan for Postpartum Hemorrhage: A Comprehensive Approach
A well-structured nursing care plan for PPH should include the following key elements:
Assessment: Gathering Vital Information
- Gather a Complete History: Assess the patient’s medical history, including previous pregnancies and deliveries, any existing health conditions, and medication use.
- Evaluate Vital Signs: Monitor blood pressure, pulse, respiration, and temperature regularly to track any changes.
- Assess for Signs of Bleeding: Observe the patient’s vaginal bleeding, including the amount, color, and consistency.
- Palpate the Uterus: Assess uterine tone, position, and tenderness.
- Monitor for Other Complications: Be alert for signs of shock, such as decreased blood pressure, fast heart rate, and pallor.
Planning: Determining the Course of Action
- Identify Goals of Care: Set goals to control bleeding, maintain vital signs within acceptable ranges, prevent complications, and promote recovery.
- Develop Nursing Interventions: Based on the patient’s condition and specific needs, plan interventions such as fundal massage, oxytocin administration, fluid replacement, and blood transfusions.
Implementation: Putting the Plan in Action
- Initiate Interventions Promptly: Implement the planned interventions in a timely and efficient manner.
- Communicate with the Physician: Keep the physician informed of the patient’s condition, any changes, and the effectiveness of interventions.
- Administer Medications as Ordered: Ensure accurate medication administration and monitor for potential side effects.
- Monitor Patient Response: Closely monitor the patient’s response to interventions and adjust the plan accordingly.
Evaluation: Assessing Progress and Outcomes
- Assess the Effectiveness of Interventions: Evaluate the effectiveness of nursing interventions in controlling bleeding, stabilizing vital signs, and preventing complications.
- Monitor for Complications: Remain vigilant for potential complications, such as infection, shock, or urinary retention.
- Document Care and Findings: Thoroughly document the patient’s condition, interventions, responses, and any changes in the care plan.
Nursing Care Plan For Postpartum Hemorrhage
Conclusion: A Collective Effort to Save Lives
Postpartum hemorrhage poses a significant risk to maternal health and well-being. A comprehensive nursing care plan, incorporating meticulous assessment, timely interventions, and proactive prevention strategies, is essential to safeguarding mothers after childbirth. By diligently employing their skills and knowledge, nurses play a pivotal role in managing this potentially life-threatening condition and ensuring a positive outcome for both mothers and their newborns. This requires unwavering commitment, collaborative effort, and a deep understanding of the complexities of postpartum hemorrhage.





