Imagine waking up one morning and struggling to see clearly. You try to adjust your glasses, but the fuzzy vision remains. Panic sets in. You realize something isn’t right. This is a scenario many individuals face when dealing with eye disorders. Nurses play a crucial role in supporting patients through these experiences, and understanding the language of nursing diagnoses is essential. This comprehensive guide will delve into the world of NANDA nursing diagnoses for eye disorders, empowering you with the knowledge to navigate these complex conditions with empathy and expertise.
Image: nandanursingdiagnosis88.blogspot.com
NANDA, or the North American Nursing Diagnosis Association, provides a standardized language that nurses use to describe patients’ health status. These diagnoses, categorized as actual, potential, or risk, help nurses develop targeted interventions and monitor patient progress. For eye disorders, NANDA diagnoses offer a framework for understanding a patient’s experience, from visual impairments and discomfort to potential complications and psycho-social distress.
Understanding the Scope of Eye Disorders
The human eye, a marvel of biological engineering, is susceptible to a wide array of conditions. These disorders can range from minor irritations to severe vision loss, significantly impacting a patient’s quality of life. To effectively care for patients with eye disorders, nurses need to possess a strong understanding of the various diagnoses that can arise. This comprehension allows nurses to provide individualized care, addressing specific needs and promoting optimal outcomes. Let’s dive into the NANDA diagnoses commonly associated with eye disorders, exploring each with depth and clarity.
NANDA Nursing Diagnoses for Eye Disorders: A Closer Look
1. Impaired Sensory Perception (Visual)
This diagnosis describes a patient’s compromised ability to receive and interpret visual stimuli. This can manifest in various ways, ranging from blurred vision to complete blindness. Causes range from refractive errors (nearsightedness, farsightedness) to more serious conditions such as diabetes-related retinopathy, glaucoma, and macular degeneration.
Causes:
- Refractive errors: These common conditions occur when the eye doesn’t properly focus light onto the retina, resulting in blurry vision.
- Cataracts: Clouding of the eye’s natural lens, leading to blurry or hazy vision.
- Glaucoma: A group of eye diseases that damage the optic nerve, which connects the eye to the brain. This can lead to peripheral vision loss and, ultimately, blindness.
- Diabetic retinopathy: Damage to the blood vessels in the retina caused by high blood sugar levels. This can lead to blurred vision, floaters, and eventual blindness.
- Macular degeneration: A condition that damages the central part of the retina, resulting in central vision loss.
Assessment:
- History and Physical: Thoroughly assess the patient’s medical history, including previous eye conditions, medications, and family history. Conduct a physical examination, paying particular attention to visual acuity, pupillary response, and eye movement.
- Visual Acuity Testing: Use a Snellen chart or similar instrument to assess visual acuity.
- Ophthalmoscopy: Use an ophthalmoscope to visualize the retina and optic nerve.
- Visual Field Testing: Evaluate peripheral vision using a perimeter or similar device.
Interventions:
- Vision Correction: Prescribe corrective lenses (glasses or contact lenses) to improve visual acuity. Consider assistive devices like magnifiers or low-vision aids.
- Medications: Administer eye drops or oral medications to manage conditions like glaucoma or diabetic retinopathy.
- Surgical Intervention: Recommend surgery for conditions like cataracts, glaucoma, or retinal detachment.
- Education and Support: Educate patients about their condition, treatment options, and self-management strategies. Provide emotional support and referral to community resources.
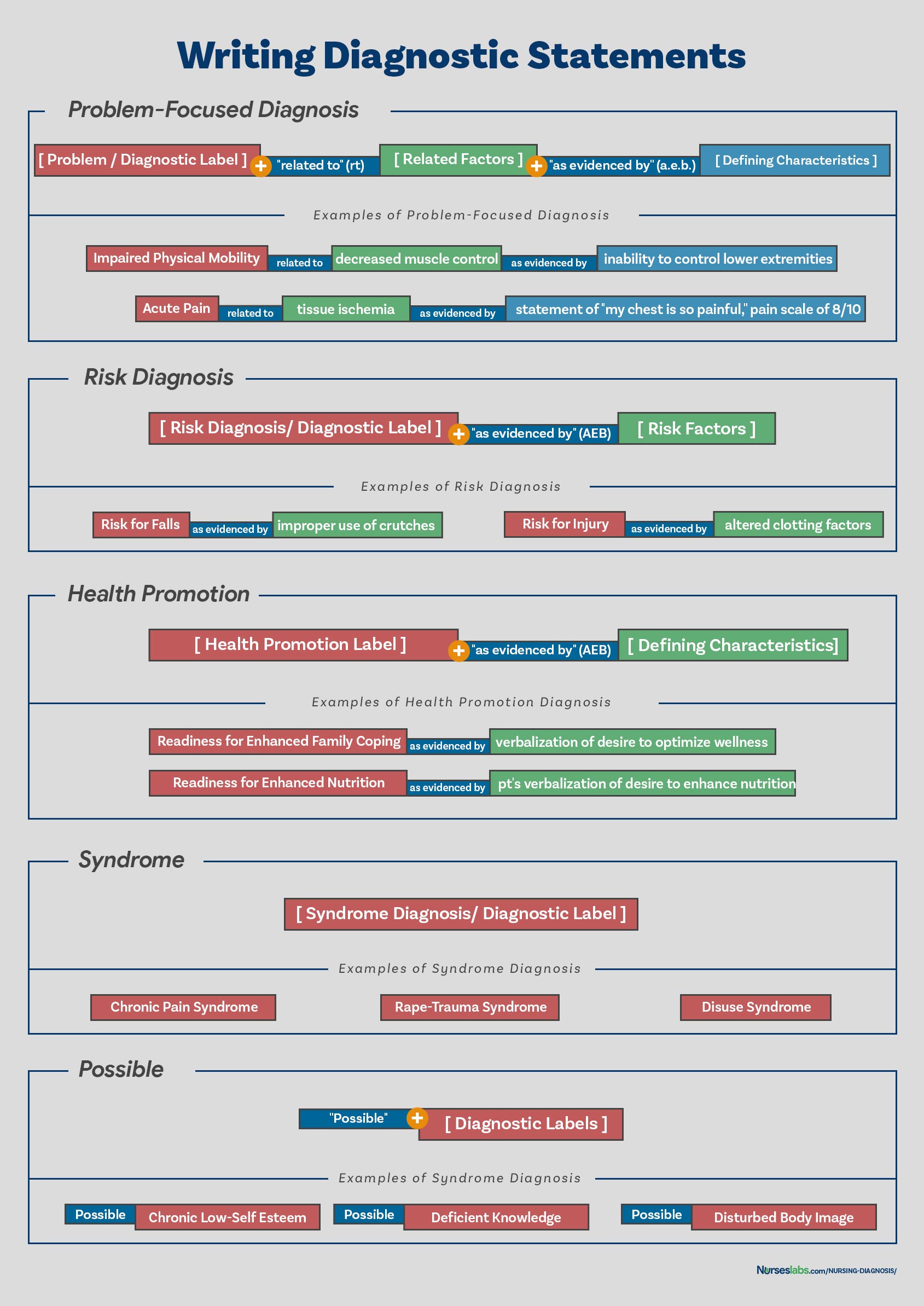
Image: webapi.bu.edu
2. Risk for Injury
Patients with eye disorders often face an increased risk of injury. This can arise from compromised vision, affecting balance and coordination, or specific conditions like corneal ulcers, which make the eye more susceptible to infection.
Causes:
- Reduced Visual acuity: Difficulty seeing clearly can lead to tripping, falling, and bumping into objects.
- Corneal ulcers: Open sores on the cornea, the clear outer layer of the eye, often caused by infections or injuries.
- Dry Eyes: Decreased tear production can make eyes more sensitive and prone to irritation.
Assessment:
- Environmental Assessment: Evaluate the patient’s home and work environments for potential hazards, such as uneven surfaces, slippery floors, and poorly lit areas.
- Fall Risk Assessment: Screen for factors that increase fall risk, including frailty, mobility limitations, and medications that can cause dizziness or drowsiness.
- Corneal Assessment: Examine the cornea for signs of injury, inflammation, or infection. Assess for dryness and discomfort.
Interventions:
- Home Safety Modifications: Suggest modifications to improve safety, such as installing grab bars, using non-slip mats, and avoiding clutter.
- Environmental Lighting: Ensure adequate lighting in the home and work environments to improve visibility.
- Protective Eyewear: Recommend wearing protective eyewear during activities with potential for eye injury, such as gardening, woodworking, or sports.
- Eye Lubrication: Encourage patients with dry eyes to use artificial tears or eye drops to lubricate the eyes.
3. Ineffective Health Maintenance
This diagnosis applies to patients who lack the knowledge, resources, or motivation to manage their eye conditions effectively. This can lead to a decline in vision and overall health.
Causes:
- Lack of Knowledge: Patients may not understand their condition, treatment options, and self-care strategies.
- Financial Constraints: Limited access to healthcare and necessary medications can hinder effective management.
- Cognitive Impairment: Memory or learning difficulties can make it challenging for patients to adhere to treatment plans.
Assessment:
- Health Literacy Assessment: Evaluate the patient’s understanding of their condition, treatment plan, and self-care instructions.
- Social Determinants of Health Assessment: Explore social factors that may influence the patient’s access to care, medication, and support services.
- Cognitive Assessment: Screen for cognitive impairment that might affect the patient’s ability to manage their condition.
Interventions:
- Patient Education: Provide clear and concise information about the patient’s condition, treatment plan, and self-care strategies. Use language and materials that are understandable to the patient.
- Support Groups: Connect patients with support groups or online resources to provide peer support and information exchange.
- Advocacy: Advocate for patients who face financial barriers to care, helping them access resources and support services.
4. Anxiety
Many patients with eye disorders experience anxiety about their vision loss and the impact it may have on their lives. This anxiety can manifest as worry, fear, and restlessness, affecting their quality of life.
Causes:
- Fear of Blindness: Anxiety about the potential for blindness and the loss of independence it represents.
- Adjustment Difficulties: Struggling to adapt to changes in daily life and activities due to decreased vision.
- Social Stigma: Fear of social stigma or discrimination associated with visual impairment.
Assessment:
- Anxiety Screening: Use validated screening tools to assess anxiety levels.
- Communication Assessment: Observe nonverbal cues and listen attentively for expressions of fear, worry, or apprehension.
- Social Support Assessment: Evaluate the patient’s social network and assess the availability of emotional support.
Interventions:
- Cognitive Behavioral Therapy (CBT): Teach coping mechanisms to manage anxiety and adjust to changes in life.
- Relaxation Techniques: Guide patients in practicing relaxation techniques, such as deep breathing, meditation, or progressive muscle relaxation.
- Support Groups: Connect patients with support groups to provide a safe space for sharing experiences and coping strategies.
Nanda Nursing Diagnosis For Eye Disorders
Conclusion
NANDA nursing diagnoses provide a valuable framework for understanding the complexities of eye disorders and their impact on patients. By understanding these diagnoses, nurses can develop comprehensive care plans that encompass physical, emotional, and social aspects of the patient’s health. It is crucial to provide patient-centered care, prioritizing individualized interventions and empowering patients to actively participate in their own healing journey. Remember, every patient deserves compassionate and competent care, allowing them to navigate the challenges of eye disorders with strength and resilience.






